Table of Contents
ToggleDiagnosing Fibromyalgia: What To Expect
Living with fibromyalgia can feel like navigating through a fog—painful, confusing, and often misunderstood. If you or a loved one suspect you might have fibromyalgia, understanding the diagnosis process can be the first step toward clarity and relief. Let’s break down what you can expect during this journey, so you’re better prepared to face it head-on.
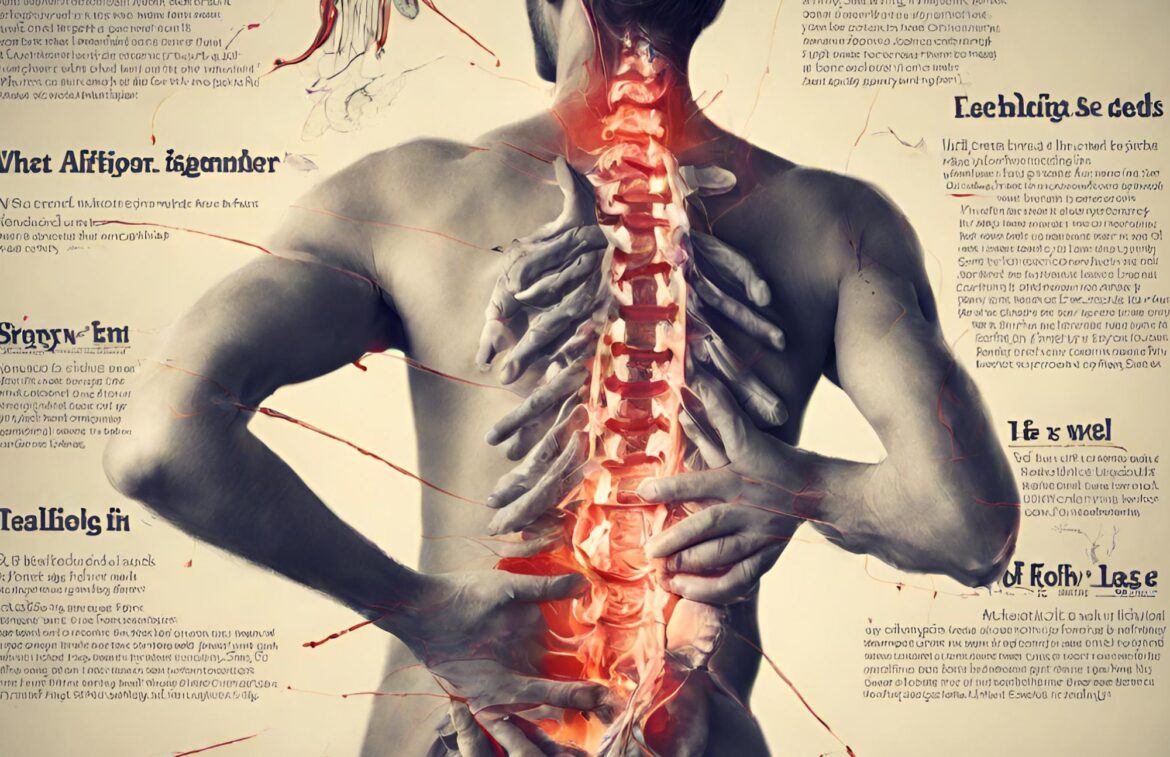
Recognizing the Symptoms
Fibromyalgia is notorious for its wide range of symptoms that can mimic other conditions. Some of the most common include:
- Widespread Pain: This pain is often described as a constant dull ache that has lasted for at least three months. It must occur on both sides of your body and above and below your waist.
- Fatigue: You may wake up tired, even though you’ve slept for long periods. Sleep is often disrupted by pain, and many patients have other sleep disorders.
- Cognitive Difficulties: Often referred to as “fibro fog,” these include problems with focus, attention, and memory.
Other symptoms can include headaches, depression, anxiety, and irritable bowel syndrome (IBS). It’s essential to keep track of what you’re experiencing, as this information will be crucial during your medical consultations.
The Diagnosis Journey
Diagnosing fibromyalgia isn’t straightforward. There’s no single test that can confirm it, which means your healthcare provider will need to rule out other conditions first. Here’s a step-by-step look at what you can expect:
1. Medical History and Symptom Discussion
Your doctor will start by asking about your medical history and symptoms. Be prepared to discuss:
- The location and intensity of your pain
- How long you’ve been experiencing symptoms
- Any other medical conditions you have
- Family history of fibromyalgia or other chronic pain conditions
2. Physical Examination
Next, your doctor will perform a physical exam to check for tenderness in specific areas of your body. These are often referred to as “tender points.” While the tender point test was once a standard diagnostic tool, it’s now considered less reliable. However, your doctor might still check these areas to get a better sense of your pain.
3. Blood Tests and Imaging
To rule out other conditions, your doctor might order blood tests or imaging studies. Common tests include:
- Complete Blood Count (CBC): To check for anemia or infection.
- Erythrocyte Sedimentation Rate (ESR): To detect inflammation in the body.
- Thyroid Function Tests: Since thyroid issues can cause similar symptoms.
- Rheumatoid Factor (RF) and Anti-Cyclic Citrullinated Peptide (anti-CCP): To rule out rheumatoid arthritis.
4. Referral to a Specialist
Given the complexity of fibromyalgia, your primary care doctor might refer you to a rheumatologist—a specialist in conditions affecting joints, muscles, and bones. Rheumatologists are more experienced in diagnosing fibromyalgia and can offer more targeted treatments.
Criteria for Diagnosis
In 2010, the American College of Rheumatology updated its criteria for diagnosing fibromyalgia. Your diagnosis might involve:
- Widespread Pain Index (WPI): A score based on the number of areas in your body where you’ve felt pain in the past week.
- Symptom Severity Scale (SSS): A score that considers the severity of your fatigue, waking unrefreshed, cognitive symptoms, and other physical symptoms.
- Duration: Symptoms must be present at a similar level for at least three months.
- Exclusion of Other Conditions: It’s important to ensure that another disorder isn’t causing your symptoms.
After the Diagnosis
Receiving a fibromyalgia diagnosis can be a mixed bag of emotions—relief that you have an answer, but anxiety about what comes next. Here’s how you can move forward:
1. Educate Yourself
Understanding your condition is empowering. Learn about fibromyalgia through reputable sources, including medical websites, books, and support groups.
2. Develop a Treatment Plan
Work with your healthcare provider to create a comprehensive treatment plan tailored to your needs. This plan might include:
- Medications: To manage pain and improve sleep.
- Physical Therapy: To increase strength and reduce pain.
- Cognitive Behavioral Therapy (CBT): To help manage the emotional impact of chronic pain.
- Lifestyle Changes: Including exercise, stress management techniques, and diet modifications.
3. Build a Support Network
Having a supportive community can make a significant difference. Connect with others who understand what you’re going through, whether through local support groups or online communities.
4. Keep a Symptom Journal
Tracking your symptoms and how different treatments affect you can provide valuable insights. Share this information with your healthcare team to fine-tune your treatment plan.
Final Thoughts
Diagnosing fibromyalgia can be a lengthy and sometimes frustrating process, but it’s a crucial step toward managing your condition and improving your quality of life. Remember, you’re not alone. Many have walked this path before and found ways to live full, vibrant lives despite fibromyalgia.
Have you recently been diagnosed with fibromyalgia? Share your experiences and tips in the comments. Let’s support each other on this journey.